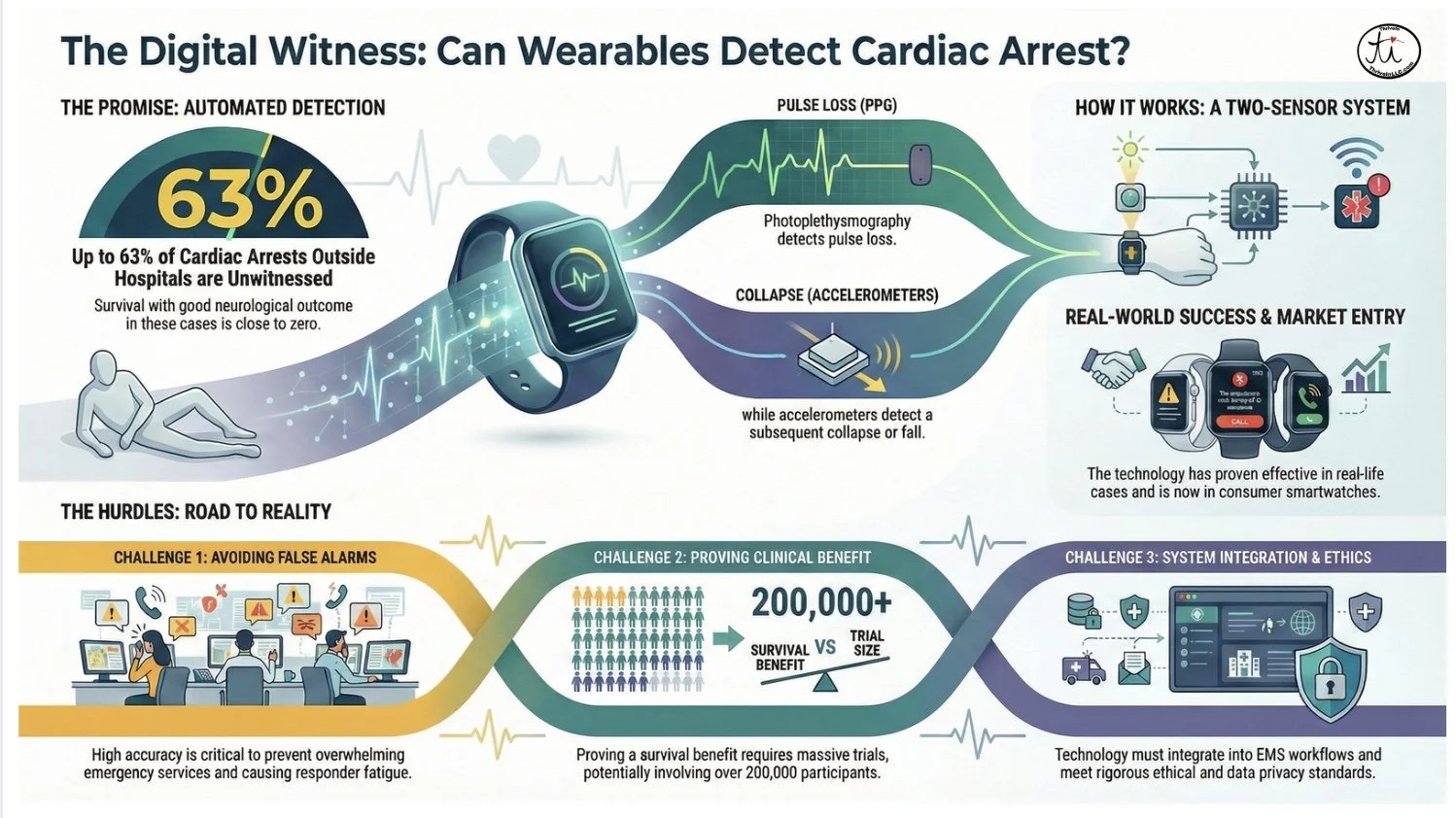
The Digital Witness: Your Smartwatch Could Save Your Life from Cardiac Arrest
We think of smartwatches as tools for convenience, tracking our steps, displaying our messages, and monitoring our workouts. But this familiar technology is quietly evolving into something far more profound. The target is one of the most critical challenges in emergency medicine: unwitnessed out-of-hospital cardiac arrest (OHCA).
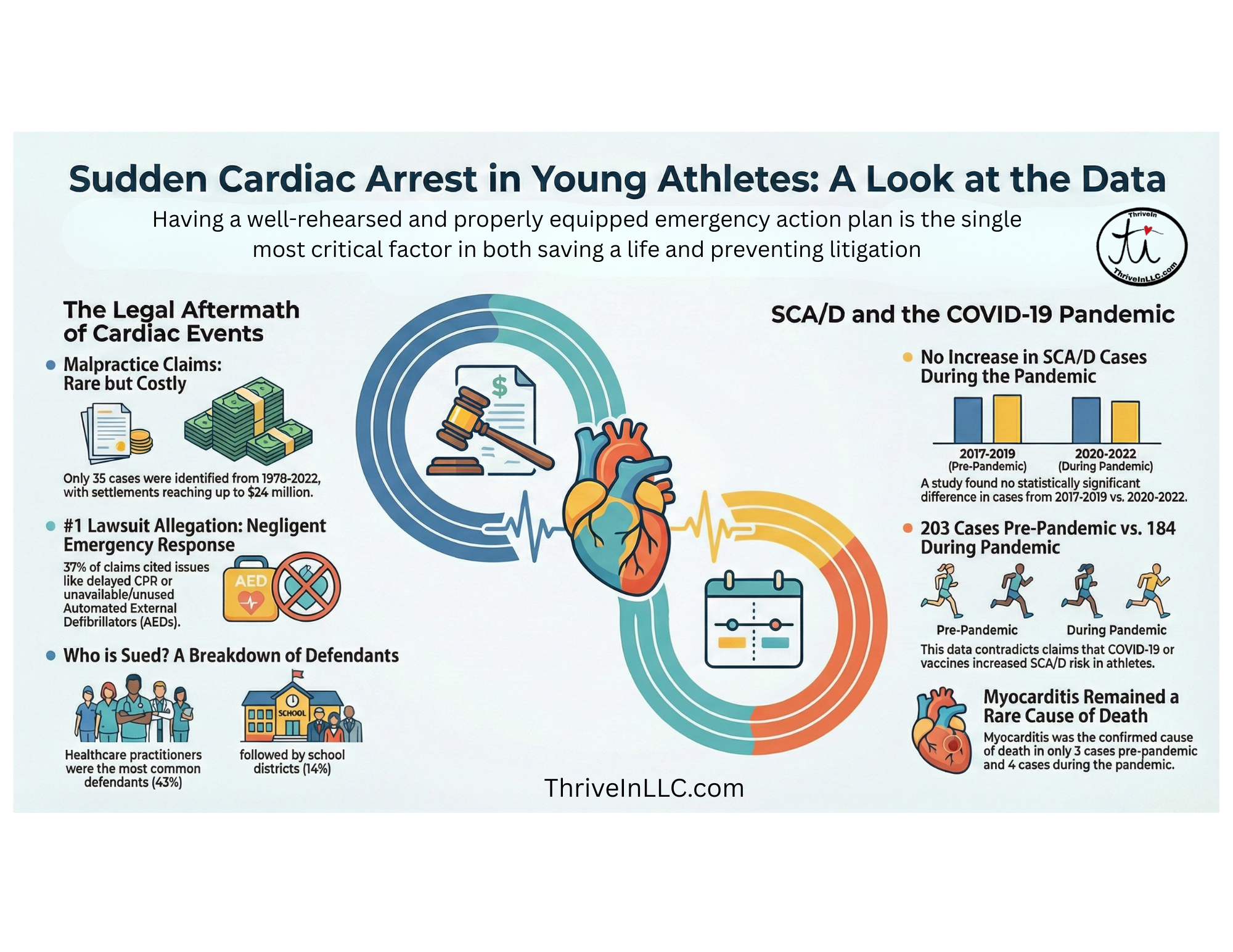
The Surprising Truths About Sudden Cardiac Arrest in Young Athletes
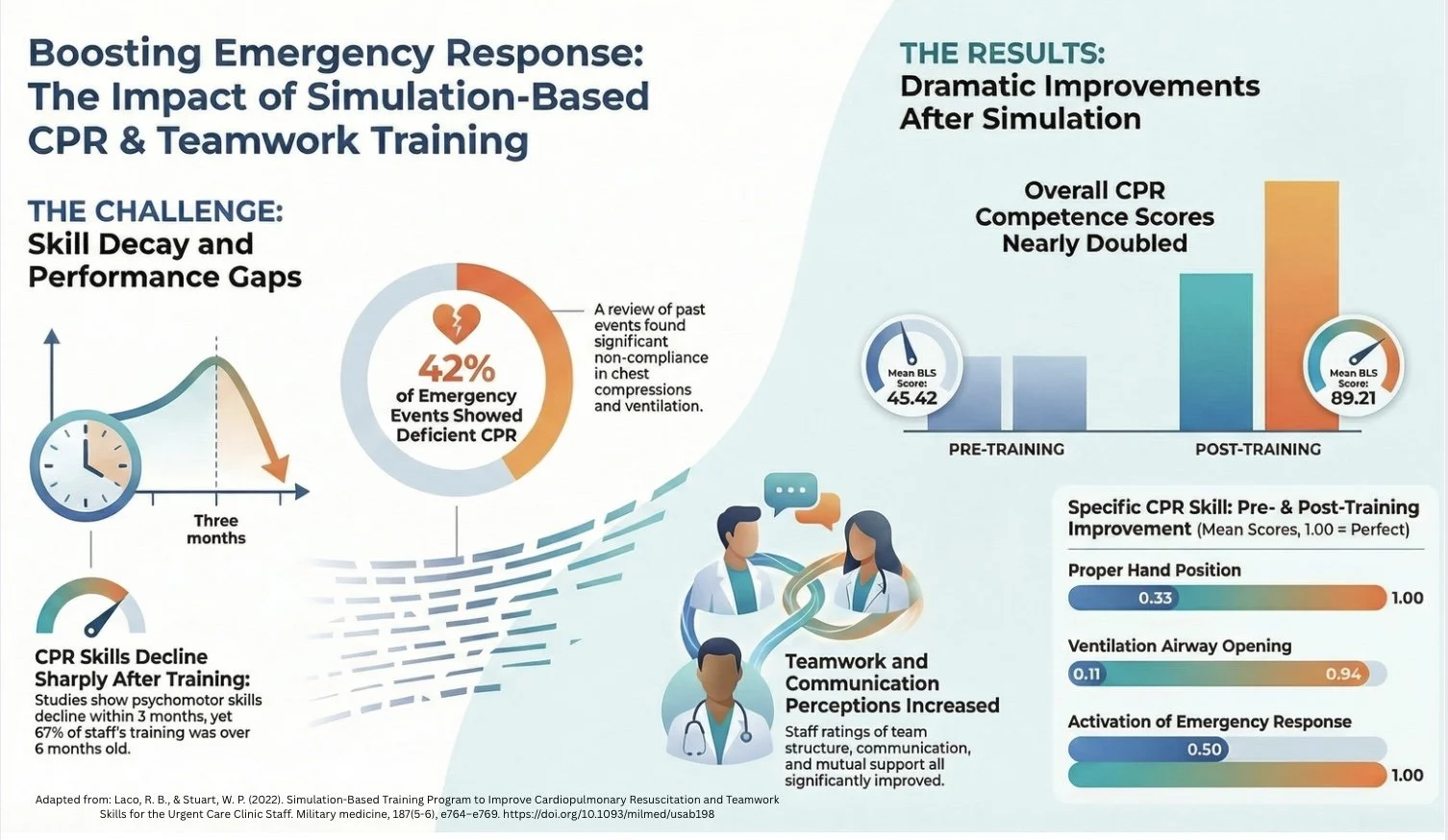
Few scenarios are more frightening for a patient or family member than a medical emergency. In those moments of crisis, we place our complete trust in the medical team, assuming every responder is flawlessly prepared to perform life-saving procedures. We expect perfection because the stakes are unimaginably high. But how do new staff get the training they need to achieve that level of skill, especially for events that are, thankfully, rare?
A Military Study Revealed the Secret to CPR Readiness in Urgent Care
How a Military Study Revealed the Secret to CPR Readiness in Urgent Care
Most people who earn a CPR certification believe they are prepared to save a life for the duration of that card, typically two years. They tuck it into their wallet, confident that should an emergency arise, they have the knowledge and skills necessary to act decisively. This certification feels like a permanent upgrade to one's personal readiness, a skill that, once learned, is always there when needed.
But a recent quality improvement project with military medical professionals challenges this core assumption. It was conducted in an Urgent Care Clinic on a military base "without immediate access to an emergency room level of services"; a setting where the stakes are incredibly high. The project revealed some counter-intuitive truths about how lifesaving skills are maintained, or more accurately, how quickly they are lost. This article breaks down the study's five most impactful takeaways.
CPR Skills Vanish Frighteningly Fast
The core finding is that CPR skills are highly perishable. Unlike riding a bike, the precise, technical motor skills required for effective CPR degrade rapidly without regular practice. The research reinforces what previous studies have found about this alarming rate of decay.
Studies have shown that CPR psychomotor skills declined 3 months and plateaued up to 6 months after the completion of CPR training.
In the study group, a majority of participants (67%) had their last CPR training more than six months prior. The full breakdown reveals a systemic gap: 11% were trained 3-6 months ago, and only 22% were trained within the last 3 months. This underscores a critical point: a one-time class every couple of years is not enough. Lifesaving skills require continuous practice to remain effective. But this rapid decay isn't the only hurdle; even recently trained professionals were found to be struggling with the absolute basics.
Even Trained Professionals Fumble the Fundamentals
Before the simulation training, a review of past emergency events at the facility showed that medical professionals had significant deficiencies in the most basic steps of CPR. This wasn't a matter of not knowing what to do, but of failing to execute properly under pressure.
The major gaps in performance were:
Activating Help: In 36% of events, staff failed to properly activate the emergency response system. This included not calling for help at all, delaying the call, or not using the overhead page correctly.
Chest Compressions: In 42% of events, chest compressions did not meet standards. Common errors included not starting quickly enough, incorrect hand placement, and performing compressions at the wrong rate or depth.
Ventilation: In 42% of events, delivering rescue breaths was done incorrectly, often due to improper airway positioning or technique.
Notice that the failure rates for activating help (36%) and teamwork (36%, as we'll see later) are identical. This suggests that communication breakdowns are just as dangerous as technical skill failures, impacting both the start of the response and its execution. This gap between theory and practice isn't just about individual memory; it's also about the environment, which is why the study's training location was so revolutionary.
Where You Train Matters as Much as How You Train
The project implemented a powerful training method called "in situ simulation training," a key driver of the program's success. This approach is defined as "simulation that occurs in the actual clinical environment and whose participants are on-duty clinical providers during their actual workday."
This is a game-changer compared to traditional CPR classes held in a generic classroom. Practicing with your actual team, in your own workspace, and using your real equipment bridges the critical gap between classroom theory and real-world application. It helps teams identify and solve logistical problems (like equipment location or communication dead zones) before a real emergency strikes, making the training intensely practical and effective.
Lifesaving is a Team Sport, Not a Solo Performance
The training program focused just as much on teamwork as it did on technical CPR skills, utilizing a framework called TeamSTEPPS (Team Strategies to Enhance Performance and Patient Safety). A review of past events found that teamwork skills were a significant weak point, with deficiencies in communication techniques like using "check-backs" and "callouts" noted in 36% of emergencies.
After the simulation training, the staff's perception of their own teamwork skills saw a statistically significant increase across four key dimensions: Team Structure, Situation Monitoring, Mutual Support, and Communication. This proves that a successful resuscitation doesn't depend on a single hero. It depends on a well-coordinated team that can communicate clearly and effectively under immense pressure.
Real-Time Feedback Drives Huge Gains
The training sessions used "high-fidelity mannequins," which are equipped with sensors that provide real-time and data-driven feedback on the most crucial CPR metrics: compression depth, rate, hand placement, and whether the provider is allowing for full chest recoil between compressions.
This immediate, objective feedback led to dramatic and rapid improvements in skill execution. Here is a look at the team's performance on key skills before and after the training, where a score of 1.00 represents perfect performance:
Correct Hand Placement: Improved from 0.33 to 1.00
Proper Airway Opening for Ventilation: Improved from 0.11 to 0.94
Allowing Full Chest Recoil: Improved from 0.55 to 0.94
To put that in perspective, a pre-training score of 0.33 for hand placement means that, on average, the medical professionals were performing this foundational step incorrectly two-thirds of the time. This is the kind of error that real-time feedback can immediately and permanently correct. The data reveals a clear lesson for any training program: objective, real-time feedback isn't a "nice-to-have"; it's the engine of rapid skill acquisition.
Practice Doesn't Make Perfect. Realistic Practice Does.
The final results of the quality improvement project were staggering. The participants' overall CPR competency score nearly doubled, jumping from a pre-simulation mean of 45.42 to a post-simulation mean of 89.21. This massive improvement wasn't the result of simply re-reading a textbook; it was the direct result of a new approach to training.
The central theme is undeniable: effective emergency readiness depends on a trifecta of training principles: frequent practice, in-situ simulation, and team-based communication. It requires practice that is as real as the event it prepares you for.
If dedicated military medical professionals in a high-stakes clinic need this level of training to stay sharp, what does that say about the rest of our readiness for an emergency?
Reference:
Laco, R. B., & Stuart, W. P. (2022). Simulation-Based Training Program to Improve Cardiopulmonary Resuscitation and Teamwork Skills for the Urgent Care Clinic Staff. Military medicine, 187(5-6), e764–e769. https://doi.org/10.1093/milmed/usab198
Are We Training New Healthcare Providers for Emergencies Wrong?
Few scenarios are more frightening for a patient or family member than a medical emergency. In those moments of crisis, we place our complete trust in the medical team, assuming every responder is flawlessly prepared to perform life-saving procedures. We expect perfection because the stakes are unimaginably high. But how do new staff get the training they need to achieve that level of skill, especially for events that are, thankfully, rare?
2-Minute CPR is Dangerously Outdated
Traditional 2-Minute CPR is Dangerous and Highly Outdated!
Patient Education Miscommunications: Conclusion
Patient Education Failures Conclusion: It's a System Problem, Not a You Problem, and ThriveIN can help!
Patient Education Miscommunications: Part 1
You walk out of the doctor's office, a handful of pamphlets and a new prescription in your bag. Your head is swimming with information about test results, lifestyle changes, and medication side effects. By the time you get home, you realize you can only recall a fraction of what the doctor said. Was it one pill a day, or two? Should you avoid salt, or was it sugar? If this experience sounds familiar, you are not alone.
Patient Education Miscommunications: Part II
Patient Education Failure #1: When the Provider Talks More, You Remember Less
Patient Education Miscommunications: Part III
Patient Education Failure #2: More Health Inequality. Information Overload Disproportionately Harms Less-Educated Patients
Patient Education Miscommunications: Part IV
Patient Education Failures #3: Proven Communication Techniques Are Rarely Used In Practice